Hysterectomy
I almost always perform a Laparoscopic hysterectomy.
There are four (4) approaches generally used to perform a Hysterectomy.
Please note that a Full Hysterectomy refers to removal of the whole uterus, which includes the cervix. It does not refer to removal of the ovaries, although this may also be performed as an additional procedure.
The method of hysterectomy which a Gynaecologist selects is usually dictated by:
the reason for surgery
size of uterus
ease of access and
the experience of the surgeon with particular techniques
Total Laparoscopic Hysterectomy (TLH) All of the surgery in this advanced laparoscopic procedure is performed through 4 small incisions in the abdomen. There is a 5mm incision at the umbilicus and a 7-8mm incision in the midline further down towards the pubic bone. There are 2 x 5mm incisions on either side of the lower abdomen. All of the suturing is performed through these incisions and so this approach is able to replace the large incision needed for a Total Abdominal Hysterectomy.
I have been performing this operation for over 15 years and now teach other interested specialists the technique.
Laparoscopically Assisted Vaginal Hysterectomy (LAVH) This is a vaginal hysterectomy in which some of the surgery is performed laparoscopically. This may include removal of the ovaries.
Vaginal Hysterectomy (VH) As the name implies, this operation is performed through the vagina and does not involve any abdominal incisions. Because of the risk of a vaginal vault haematoma, many surgeons will perform a laparoscopy in order to check this area at the end of the operation. In addition, a cystoscopy (look inside the bladder) is often performed to exclude an injury to the ureters which connects the kidney to the bladder. These structures are always at risk of injury during a hysterectomy as they pass very close to the cervix. Many women who are able to have a vaginal hysterectomy will also have prolapse and therefore a vaginal hysterectomy may often be combined with a repair of the anterior (front) and or posterior (back) vaginal walls.
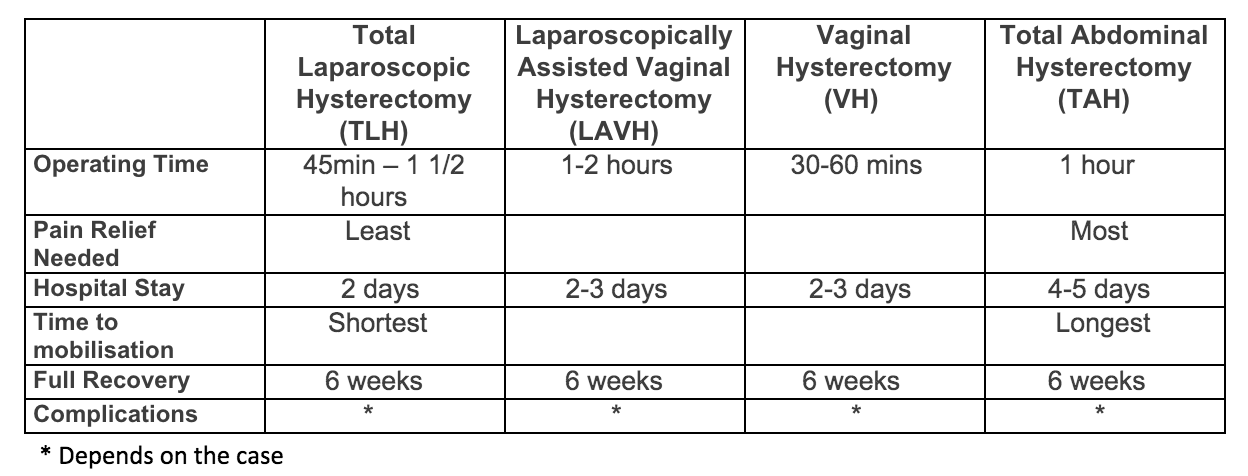
In brief, the methods compare as follows:
Regardless of the method by which a hysterectomy is performed, each operation requires division of the same structures and the rebuilding of support for the vaginal vault (top of the vagina). For this reason, full recovery is always six weeks and women often feel tired during that time and potentially for around three months after surgery. The method of surgery will determine how rapidly you will return to normal activities including walking, cooking, driving and general mobilisation around the home.
Complications : Any operation may have complications and certain complications are specific to or more common with particular procedures. For instance, a collection of blood (haematoma) at the top of the vagina is more common after a Vaginal Hysterectomy (VH) and wound infections are more common with large incisions found in Abdominal Hysterectomy (TAH).
A full list of recognised complications of Hysterectomy is too extensive to place here, but some of the better known are:
Bleeding requiring transfusion (notify your doctor if you are taking aspirin, anti-inflammatory agents such as Ibuprofen or any herbal remedy such as glucosamine or fish oil)
Wound infection
Deep vein thrombosis
Bladder injury
Vascular injury
Ureteric injury (connects kidney to bladder)
Vault haematoma
Urinary tract infection
Weird Things That Can Happen
Adhesions: These can occur after any surgery but are generally less common with Laparoscopic procedures. With any hysterectomy, small or large bowel may become adherent to the top of the vagina in the weeks following the operation. This is more likely to happen if there is bleeding (vault haematoma) or infection.
Adhesions cannot be completely prevented, and some patients appear to be more prone to developing these than others. Further surgery can be required to divide the adhesions.
Bleeding after Hysterectomy:
Early, due to evacuation of a haematoma at the top of the vagina. This will usually happen within 10-14 days of surgery
Late, due to vascular healing tissue called granulation tissue at the vault. This is relatively common and may not present until sex is resumed, at which time some bleeding and sensitivity will be noticed. Silver nitrate is used to chemically cauterize this tissue. If there is a large amount of this tissue, it may need to be removed in theatre.
Pre-operative Care: It is important to make sure you are not constipated prior to surgery, as the drugs used for pain relief can make this much worse. Coloxyl, agarol, metamucil and plenty of fluids in the week prior to surgery can make a big difference to your recovery.
Postoperative Care: Naturally, the care which you receive following your surgery will depend to a certain extent on the type of procedure which you have.
Abdominal incisions will be covered with dressings which are removed after 24-48 hours. Sometimes sutures pass through small vessels in the skin and these can ooze overnight causing dressings to look very bloodstained.
If you have a vaginal hysterectomy, then there may be a pack in the vagina to minimise blood loss. This is usually removed the next morning but can cause some discomfort overnight. Regardless of your procedure, vaginal loss is monitored following a hysterectomy.
Depending on how you feel, you will be mobilised the day after surgery in order to minimise your risk of deep vein thrombosis and to assist your general recovery. All patients will have a catheter in the bladder which will be removed, in most cases, the next morning. Drips are also taken out the next day but may be left if they are also providing access for antibiotics or pain relief. Some patients will have a drain coming through the abdominal wall and this is usually removed after 24 hours.
Constipation should be treated vigorously pre and post operatively. Use something to keep the bowels flowing smoothly (eg Metamucil).